From the Editor
Why is breast density a weighty matter?
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...
Wendie A. Berg, MD, PhD; JoAnn Pushkin; and Cindy Henke-Sarmento
Dr. Berg is Professor of Radiology, University of Pittsburgh School of Medicine, Magee-Womens Hospital of UPMC, Pittsburgh, Pennsylvania, and Chief Scientific Advisor, DenseBreast-info.org.
Ms. Pushkin is Executive Director, DenseBreast-info, Inc.
Ms. Henke-Sarmento is Technology Director, DenseBreast-info, Inc.
Ms. Pushkin and Ms. Henke-Sarmento report that the 501(c)(3) nonprofit, DenseBreast-info, Inc., which supports the Web site DenseBreast-info.org, has received unrestricted educational grants from GE Healthcare and Volpara Solutions Ltd. Dr. Berg reports no financial relationships relevant to this article.

An expert radiologist and dense breast educators address specific questions that will arise in your counseling and care of women who are identified with dense breasts on mammography
In this Article
It’s a movement that shows no signs of abating. Women in 24 states, encompassing 67% of American women, now receive some level of notification after their mammogram about breast density. Individual patient advocates continue to push for notification, and states are likely to continue to draft bills. On the national level, a federal standard is being pursued through both federal legislation and federal regulation. Clinicians practicing in states with an “inform” law, either already in effect or imminent, will be tasked with engaging in new patient conversations arising from density notification. Are you ready to answer your patients’ questions?
Navigating inconsistent data and expert comments about density and discerning which patients may benefit from additional screening can create challenges in addressing a patient’s questions about the implications of her dense tissue. If you feel less than equipped to address these issues, you are not alone. A recent survey of clinicians, con- ducted after California’s breast density notification law went into effect, showed that only 6% were comfortable answering patients’ questions relating to breast density. Seventy-five percent of respondents indicated they wanted more education on the topic.1
For women having mammography, dense breast tissue is most important because it can mask detection of cancers, and women may want to have additional screening beyond mammography. Women with dense breasts are also at increased risk for developing breast cancer. For clinicians who are on the front lines of care for women undergoing screening, the most important action items are:
To assist you in informing patient discussions, in this article we answer some of the most frequently asked questions of ObGyns.
Which breasts are considered dense?
The American College of Radiology recommends that density be reported in 1 of 4 categories depending on the relative amounts of fat and fibroglandular tissue2:
Breasts that are either heterogeneously dense or extremely dense are considered “dense.” About 40% of women older than age 40 have dense breasts.3
This patient has heterogeneously dense breast tissue. Standard 2D mediolateral oblique (MLO) digital mammogram (A) and MLO tomosynthesis 1-mm slice (B) reveal subtle possible distortion (arrow) in the upper right breast. On tomosynthesis, the distortion is better seen, as is the underlying irregular mass (red circle).
Ultrasound (US) directed to the mass (C) shows an irregular hypoechoic (dark gray) mass (marked by calipers), compatible with cancer. US-guided core needle biopsy revealed grade 2 invasive ductal cancer with associated ductal carcinoma in situ.
Axial magnetic resonance imaging of the right breast obtained after contrast injection, and after computer subtraction of nonenhanced image (D), shows irregular spiculated enhancing (white) mass (arrow) due to the known carcinoma.
Images: Courtesy Wendie Berg, MD, PhD
Who needs more screening?
The FIGURE is a screening decision support tool representing the consensus opinion of several medical experts based on the best available scientific evidence to optimize breast cancer detection.
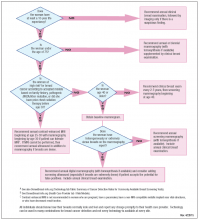
This flow chart was developed as an educational tool by DenseBreast-info.org and reflects the consensus opinion of the educational Web site’s medical reviewers based on the best available scientific evidence. The proposed strategy is relatively aggressive, designed to optimize cancer detection. Other guidelines may recommend a later start or different screening frequency. This is not intended to be a substitute for medical advice from a physician or to create a standard of care for health care providers. Please check DenseBreast-info.org for updates to this flow chart. Copyright DenseBreast-info, Inc.
Do dense breasts affect the risk of developing breast cancer?
Yes. Dense breasts are a risk factor for breast cancer. According to the American Cancer Society’s Breast Cancer Facts & Figures 2013−2014, “The risk of breast cancer in-creases with increasing breast density; women with very high breast density have a 4- to 6-fold increased risk of breast cancer compared to women with the least dense breasts.”4,5
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...
The benefit is small and the cost is high, according to this comparative modeling study.

The authors of this prospective study involving more than 350,000 patients observed high interval cancer rates for women with 5-year breast cancer...
