
- Placement of TVT-O transobturator tape
- Monarc transobturator procedure
- TVT Exact retropubic sling operation
These videos were selected by Mark D. Walters, MD, and presented courtesy of the International Academy of Pelvic Surgery (IAPS).
Only 15 years ago, when surgery was recommended for patients who had bothersome stress urinary incontinence (SUI), they were offered operations such as suburethral (Kelly) plication, needle urethropexy, open or laparoscopic Burch procedure, and pubovaginal fascial sling procedure. Today, virtually all of these operations have been replaced in general practice by retropubic or transobturator (TOT) midurethral synthetic slings.
Although Burch colposuspension and the pubovaginal fascial sling procedure are effective for both primary and recurrent SUI, they are more invasive than midurethral slings, cause more voiding dysfunction, and have significantly longer recovery times, making them less attractive for most primary and recurrent cases of SUI.
The evolution of SUI surgeries has shifted so far toward midurethral slings that Burch colposuspension and the pubovaginal sling procedure are rarely performed or taught in obstetrics and gynecology or urology residency programs; these procedures are now mostly done in fellowship programs by specialists in female pelvic medicine and reconstructive surgery.
In this article, we describe how an ObGyn generalist can approach the surgical treatment of women who have either primary or recurrent SUI. Using evidence-based principles, when available, we also discuss how different clinical characteristics—as well as the characteristics of the available slings—affect the suitability of the sling for individual patients.
One caveat: This article assumes that the surgeon knows how to, and is able to, perform retropubic and TOT sling procedures equally well. However, when this is not the case, the surgeon should perform the sling procedure that she or he does best, assuming that it is appropriate for that particular patient.
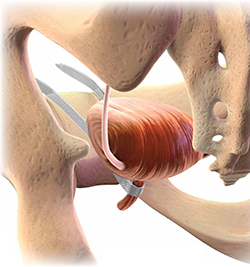
Almost all surgical procedures for stress urinary incontinence performed today involve placement of a retropubic or transobturator midurethral synthetic sling.
Illustration: Craig Zuckerman for OBG Management
CASE: SUI and Stage II anterior vaginal prolapse
A healthy 45-year-old G2P2 woman complains of a 5-year history of worsening SUI symptoms, mostly occurring during activities such as coughing, laughing, and running. The incontinence has become so severe that she requires several pads daily. She is able to void without difficulty or pain, and her bowel movements are normal. She has regular menses, has had a tubal ligation, and is sexually active.
She reports that she has been performing daily Kegel pelvic muscle exercises, without improvement.
On physical examination, she is found to have Stage II anterior vaginal prolapse and urethral hypermobility, with normal uterine and posterior vaginal support. The uterus and ovaries are of normal size.
A full bladder stress test in the office reveals immediate loss of urine from the urethra upon coughing in a semi-sitting position. She voids 325 mL after the examination and has a post-void residual urine volume, as measured by ultrasonography (US), of 25 mL. Urinalysis is negative.
When discussing her goals, the patient expresses a desire for a cure of her urinary incontinence, if possible.
What further testing and treatment options do you offer to her?
If you and the patient agree that surgery is warranted, which procedure do you recommend?
Recommended assessment of women who report SUI
Women who have bothersome urine loss during activities such as exercise, coughing, or laughing should undergo a history, physical examination, and urinalysis. During the pelvic examination, it is important to assess pelvic organ support defects, especially those involving the anterior vagina and urethra. Also note levator ani muscle contraction and strength. In addition, you can use this time to discuss whether the patient is doing, or has done, pelvic muscle (Kegel) exercises; teach the exercises, if necessary; and encourage her to do them in the future.
If the patient has no urinary infection, has performed Kegel exercises without further benefit, and wishes to consider surgical treatment, basic assessment of lower urinary function is indicated. Basic office urodynamic testing includes:
- a measured void
- measurement of post-void residual volume (by catheter or US)
- assessment of bladder sensation and capacity
- provocation for overactive bladder
- a full-bladder cough stress test (a positive test is direct observation of urethral loss of urine upon coughing).
Patients who have a complex history or mixed symptoms, previous failed surgery, or other characteristics that suggest a diagnosis other than simple SUI should undergo formal electronic urodynamic testing.1
Patient selection criteria
Primary sling surgery is an option for patients who have:
- no urinary infection
- normal voiding and bladder-filling function
- urethral hypermobility on examination
- SUI on a cough-stress test
- failure to improve sufficiently with pelvic muscle exercises.



