What is urinary incontinence?
Urinary incontinence is a condition in which a person unintentionally leaks urine. She may uncontrollably urinate when she laughs, coughs, or exercises. Or she may find she cannot wait to reach the bathroom. These problems, which may be temporary or permanent, can be caused by a number of conditions, including urinary tract infections, bladder weakness, or a blocked urethra (the canal that transports urine from the bladder).
Is urinary incontinence common?
Yes, it is very common, especially among women. Seventeen million people in the United States experience incontinence at some point in their lives, and approximately 10% to 30% of women between the ages of 15 and 64 have this problem. That number may be even higher, since many women with incontinence are too embarrassed to seek treatment.
Does urinary incontinence affect only elderly women?
Bladder control problems are not a natural part of the aging process and can affect women of all ages.
Is all urinary incontinence the same?
No, there are several different types of this condition:
- Stress incontinence. Women with stress incontinence may leak urine when they exercise, cough, sneeze, laugh, lift, or put pressure on their abdomen. This often is due to weakness in pelvic floor muscles and may be caused by childbirth or pelvic surgery.
- Urge incontinence. This condition, sometimes referred to as “overactive bladder,” is the most common form of incontinence. It may cause women to lose urine as soon as they drink a small amount of liquid or have the urge to go to the bathroom. It also may result in frequent urination (every half hour, for example) or bedwetting.
- Mixed incontinence. Patients with this condition suffer from both stress and urge incontinence.
- Overflow incontinence. Women with overflow incontinence may feel like they never completely empty their bladders. Some may pass only a small amount of urine and feel like their bladder is still full. Others may feel as if they have to empty their bladders but can’t.
- Functional incontinence. Women with functional incontinence cannot get to the toilet or use a bedpan in time to urinate. The urinary system works, but physical or mental disabilities prevent normal bathroom use.
- Transient incontinence. This is temporary incontinence that occurs due to certain conditions, including urinary tract infections, the use of some medications, and restricted mobility.
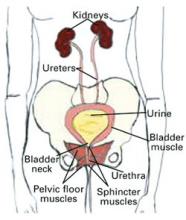
Normal urine flow. Urine is produced in the kidneys, then travels through the ureters to the bladder, where it is stored. During urination, the urethra carries the urine outside of the body.
Are there tests for incontinence?
If you think you have urinary incontinence, schedule an appointment with your doctor. He or she will talk to you about your medical history and urinary habits, and may perform a physical examination as well as a urine test. Other tests will help find the cause of your incontinence and the best treatment for you (see “What can I expect during a urinary incontinence test?”).
- Pad test: You’ll wear a pad for up to 2 hours, then place it in a sealed plastic bag. A health-care provider will weigh the bag to see how much urine the pad is holding.
- Cystoscopy: Your physician will look for abnormalities in your bladder and lower urinary tract by inserting a small telescopic tube into your bladder.
- Postvoid residual measurement: A small, soft tube or an ultrasound is used to measure the amount of urine left in your bladder after you’ve gone to the bathroom.
- Stress test: Your doctor will ask you to cough, lift, or exercise to see if any of these activities cause you to lose urine.
- Urinalysis: A clinician will examine your urine for any signs of infection, blood, or other abnormalities.
- Uroflowmetry: This measures urine speed and volume. Special equipment is used to show any changes in the flow rate.
- Urodynamics testing: Your doctor will take a closer look at the filling and emptying process by placing pressure-measuring instruments in the bladder.
Is incontinence treatable?
There are many treatment options available for urinary incontinence. Speak with your doctor to find out if one is right for you.
Nonsurgical treatments
- Pelvic muscle exercises—also called Kegel exercises—help strengthen weak muscles around the bladder.
- Bladder training can help you resist the urge to urinate by having you go to the bathroom only at certain, designated times.
- Medications can influence bladder contraction and improve the tension of certain muscles and the urethra.
Surgical treatments
- Slings—made of mesh tape or a person’s own tissue—are used to restore support to the bladder neck, which allows the bladder to hold urine.
- Bladder neck suspension is a procedure in which a doctor places stitches in the wall of the vagina, beside the urethra, to provide extra support.