- Stop staring at that Category-II fetal heart-rate tracing…
Robert L. Barbieri, MD (Editorial, April 2011) - Guidelines on fetal monitoring aim to codify normal, abnormal FHR
Robert L. Barbieri, MD (Editorial, October 2008)
CASE An uncertain interlude during labor
An obstetrician checks on her laboring patient, only to discover that the fetal heart-rate (FHR) tracing has moved from Category I, a normal classification, into Category II—a gray zone. The OB decides to be proactive, not simply to wait for the tracing to return to normal. She has the patient move from a supine to a lateral position, provides oxygen, and administers a bolus of 500 to 1,000 mL of lactated Ringer’s solution over 20 minutes.
The tracing remains in Category II.
What should the OB do next?
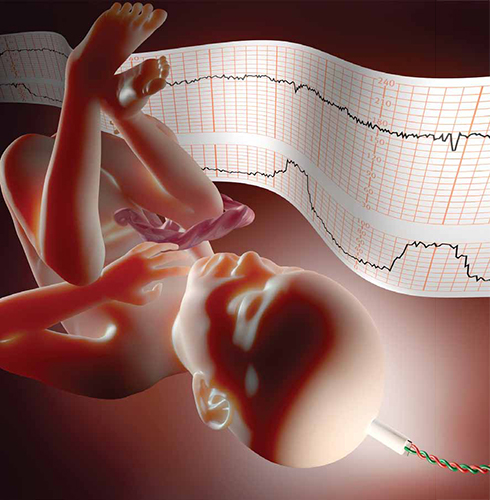
When a fetal heart-rate tracing remains in Category II despite well-considered conservative corrective measures, a reasoned, rather than passive, approach is recommended.In 2008, the National Institute of Child Health and Human Development proposed a three-tier classification system for electronic FHR tracings (TABLE 1).1 Tracings in Category I are considered normal and can be managed routinely.1-3 Category-III tracings are considered abnormal and require additional attention; if corrective measures do not result in improvement, rapid delivery usually is warranted.1-3 Category II includes all FHR tracings that do not fit into either of the other categories. Because Category II encompasses such a wide range of FHR tracings, there are many options for management.
TABLE 1
3-tier fetal heart-rate classification system
| Category | Description |
|---|---|
| I | Fetal heart-rate (FHR) tracings include all of the following:
|
| II | Includes all FHR tracings not included in Category I or Category III |
| III | FHR tracings include:
|
| Source: Adapted from Macones GA, et al.1 | |
If the case described above sounds familiar, it may be that you read Editor in Chief Dr. Robert L. Barbieri’s editorial on Category-II FHR tracings in the April 2011 issue of OBG Management.4 That essay described a number of common conservative corrective measures applicable for Category-II tracings, including the three interventions the OB performed.
Other measures:
- reduce or stop infusion of oxytocin
- discontinue cervical ripening agents
- consider administering a tocolytic, such as terbutaline, if tachysystole is present or if uterine contractions are prolonged or coupled
- consider the option of amnioinfusion if variable decelerations are present.4,5
Systematic review of the oxygen pathway, from the environment to the fetus (maternal lungs, heart, vasculature, uterus, placenta, and umbilical cord), can facilitate recollection of all of these measures. In addition, a simplified “A-B-C-D” approach to the management of a Category-II FHR tracing is helpful (TABLES 2 and 3):
- Assess the oxygen pathway
- Begin conservative corrective measures
- Clear obstacles to rapid delivery
- Determine decision-to-delivery time.6,7
TABLE 2
Conservative corrective measures to improve fetal oxygenation
| “A” Assess oxygen pathway | “B” Begin corrective measures if indicated | |
|---|---|---|
| Lungs | Airway and breathing | Supplemental oxygen (10 L) using a tight-fitting, non-rebreather face mask for at least 15 minutes |
| Heart | Heart rate and rhythm | Position changes IV fluid bolus (500–1,000 cc of isotonic fluid over 20 min) Correct hypotension |
| Vasculature | Blood pressure Volume status | |
| Uterus | Contraction strength Contraction frequency Baseline uterine tone Exclude uterine rupture | Stop or reduce uterine stimulants (oxytocin, prostaglandin) Consider uterine relaxant (terbutaline) |
| Placenta | Placental separation Bleeding vasa previa | |
| Cord | Vaginal exam Exclude cord prolapse | Consider amnioinfusion |
| Courtesy of David A. Miller, MD | ||
As the obstetrician in the opening scenario knows all too well, conservative corrective measures do not always transform FHR tracings from Category II to Category I. In fact, it is extremely common for a Category-II tracing to remain in Category II despite every conservative corrective measure in the book. This article presents a practical, systematic, standardized approach to the management of a persistent Category-II FHR tracing.
TABLE 3
Steps involved in preparing for delivery
| “C” Clear obstacles to rapid delivery | “D” Determine decision-to-delivery time | |
|---|---|---|
| Facility | Operating room availability Equipment | Facility response time |
| Staff | Notify: Obstetrician Surgical assistant Anesthesiologist Neonatologist Pediatrician Nursing staff | Consider staff: Availability Training Experience |
| Mother | Informed consent Anesthesia options Laboratory tests Blood products Intravenous access Urinary catheter Abdominal prep Transfer to OR | Surgical considerations (prior abdominal or uterine surgery) Medical considerations (obesity, hypertension, diabetes, SLE) Obstetric considerations (parity, pelvimetry, placental location) |
| Fetus | Confirm: Estimated fetal weight Gestational age Presentation Position | Consider factors such as: Estimated fetal weight Gestational age Presentation Position |
| Labor | Confirm adequate monitoring of uterine contractions | Consider factors such as: Arrest disorder Protracted labor Remote from delivery Poor expulsive efforts |
| Courtesy of David A. Miller, MD | ||
CASE Continued
When the OB’s preliminary interventions fail to nudge the FHR tracing back to Category I, she stops oxytocin and administers terbutaline. She even tries amnioinfusion. Still, the FHR tracing remains in Category II.



