You are performing the fourth cesarean delivery on your patient, a 30-year-old G4P3. The abdominal and uterine incisions go well, and delivery is uneventful. As you prepare to close the uterus, you notice that there is a hole in the bladder 5 cm long. You realize that the injury likely occurred before you made the uterine incision, at the time you mobilized the bladder from the lower uterine segment.
Now, how will you repair the injury to the bladder?
Injury to the bladder or ureter occurs in about 0.3% of cesarean deliveries and about 1% of gynecologic surgical procedures. Bladder injury is more common than injury to the ureter.1,2
Intraoperative recognition of the injury usually permits prompt and successful repair. Delayed recognition of the injury—in the postoperative period—is associated with serious complications, however.
Preoperative planning—that ounce of prevention
Risk factors for cesarean-related bladder injury include:
- repeat delivery
- emergency delivery
- delivery after a protracted second stage of labor.
Bladder injury has been reported to occur in about 0.2% of primary cesarean deliveries and in 0.6% of repeat cesarean deliveries.3
During repeat cesarean delivery, two surgical challenges are often encountered: The bladder 1) is densely adherent to the underlying lower uterine segment and 2) might have healed in a position much higher on the uterus, thereby blocking access to the lower uterine segment.
During emergency cesarean delivery for placental abruption or fetal bradycardia, bladder injury might occur because visualization and dissection of each surgical plane is less than optimal.
In cesarean delivery after a protracted second stage, the vagina—rather than the lower uterine segment—might be incised because of difficulty identifying the interface between uterus and vagina, resulting in an increased risk of bladder injury.
Tips. You can reduce the risk of injury to the bladder as follows:
- Enter the peritoneal cavity at the most superior segment of the abdominal incision; use sharp, rather than blunt, dissection to separate a densely adherent bladder from the uterus.
- When your patient is carrying a large fetus and experiencing a prolonged second stage of labor—and requires cesarean delivery—consider performing a low vertical uterine incision to reduce the risk of extensions into the broad ligament.
Repairing injury to the dome
The bladder comprises the dome superiorly and the base inferiorly. The base of the bladder contains the trigone, which includes the ureters that enter posteriorly and the urethra that exits at the most inferior portion of the bladder (see the FIGURE).
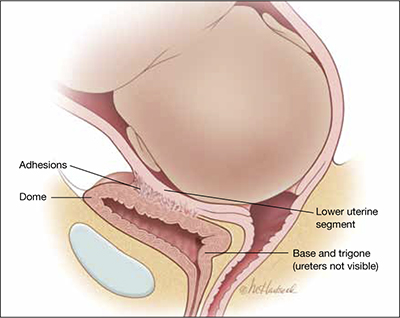
The bladder at delivery: Position and parts
During cesarean delivery, most injuries to the bladder occur in the dome, far from the trigone.During cesarean delivery, most injuries to the bladder occur in the dome, far from the trigone. You can demonstrate this by trying to feel the tip of the Foley catheter bulb through a bladder injury that occurs during cesarean delivery: The trigone is, typically, more than 6 cm—and often more than 10 cm—distant from injury in the dome.
ObGyns are highly qualified to repair an injury in the dome. The surgical steps often used to repair cystotomy in the dome of the bladder include:
- Identify the extent of injury; ensure that it is limited to the dome (that is, does not involve the trigone or is not a large one that extends deep into the posterior bladder).
- Repair the cystotomy in two layers, using absorbable suture. Never use non-absorbable suture because it might act as a nidus for bladder calculi to form. Close the first layer with simple running 3-0 absorbable suture. Close the second layer using running imbricating 2-0 or 3-0 absorbable suture.
- To ensure integrity of the repair and to detect the presence of any other bladder injuries, backfill the bladder with a sterile milk or indigo carmine dye through the Foley catheter.
- The bladder should be drained by Foley catheter for approximately 7 days.
Repairing injury to the trigone or ureters
In most cases, an urologist or urogynecologist should be called in to repair an injury to the trigone or ureter. A possible exception: When it is clear that a stitch has kinked one of the ureters, and removing that stitch resolves the problem.
If you detect a large injury to the bladder—one that involves the posterior wall—consider that the trigone might be injured. Repair of the bladder should then be delayed until a ureteral dye test can be performed.
Ureteral dye test. Inject 5 mL of indigo carmine dye intravenously, and directly observe the flow of dye-stained urine from both ureteral orifices. If you see that dye is flowing from both ureteral orifices and you do not see dye in the retroperitoneal and intra-abdominal spaces, ureteral integrity is likely and you can proceed to repair the injury to the dome.


