“A STEPWISE APPROACH TO CERVICAL CERCLAGE”
KATRIN KARL, MD; MICHAEL KATZ, MD (JUNE 2012)
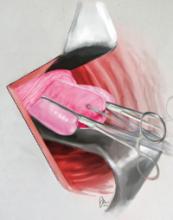
Confused by cover illustration of cerclage
I keep looking at the illustration on the cover of the June issue to try to identify the anatomic elements grasped by the clamps. Is this a view into the vagina looking at the external os, and the cervix is grasped to place the cerclage—what anatomic landmarks are those? Am I confused or just ignorant?
Federico G. Mariona, MD
Dearborn, Michigan
Dr. Katz responds Illustration shows clamped epithelium in cerclage from an unusual position
I am delighted to hear from Dr. Mariona, and can assure him that he is NOT ignorant. I can very easily understand how the artist’s rendering illustrating the cervical cerclage article could possibly cause confusion. My apologies.
Dr. Mariona is probably wondering about those “appendages” on both sides of the Allis clamps. The “appendages” are formed when the clamps cinch the epithelial tissue on either side of the cervix.
Using a silicone model, I have created a short VIDEO* to show how this has come about. The model, which I use for teaching, has the following features: a blue line on top to delineate the cervico-vesical plica, a pink colored core (stroma), and a soft tissue covering the stroma representing the cervical epithelium or mucosa. In my model, the epithelium is only 2–3 mm thick all around; in some patients, it is well above 5–10 mm thick and wider than the cervical stroma by far.
FIGURE 1 provides two photographs of how the clamped epithelium appears from different angles before and after tying the knot. The angle you see in the June cover illustration is simply looking at it straight from the front—a little unusual and potentially confusing.
FIGURE 1 “Appendages” formed by clamped epithelial tissue
Both sets of Allis clamps have been placed on a silicone model, creating an “appendage”
of epithelial tissue on both sides of the cervix. (A) is a view from the side of the cerclage;
(B) from the top and front. The model has a blue line on top to delineate the cervico-vesical
plica, a pink-colored core or stroma, and a soft tissue covering that represents the cervical
epithelium or mucosa.FIGURE 2, which was deleted from the original article because of space limitations, also gives a good perspective from the top.
FIGURE 2 Clamping the cervical epithelium
Using bilateral Allis clamps, the soft tissue covering the core (stroma) is clamped between the cervico-vesical junction anteriorly and the superior point of the posterior fornix, posteriorly. This cardinal step separates the core from the mucosal/submucosal elements.The article discusses clamping the soft tissue covering the cervical core or stroma in Step 5 and Figure 6 on page 35.
“DOES ELIMINATION OF THE BLADDER FLAP FROM CESAREAN DELIVERY INCREASE THE RISK OF COMPLICATIONS?”
BAHA M. SIBAI, MD (JUNE 2012)
Making the incision well above the bladder reflection is crucial
I don’t think trying to decide whether to create a bladder flap or not is the issue. Making the uterine incision well above the bladder reflection is what’s important.
A more useful study is to compare bladder injury and/or time of procedure in patients who have the bladder flap closed (usually above the uterine scar). It still makes no sense to me when I do repeat cesarean sections and find the bladder tacked up to the uterus, usually well above the prior closure. It’s even a bigger problem in the event of a dehiscence, when the main chore is to safely peel away the bladder from “tissue paper” uterine wall to ensure proper uterine closure.
Better yet, STOP closing the bladder flap.
Miguel A. Cano, MD
Reedley, California
“BE ACTIVE, NOT PASSIVE, WITH HOW YOU SCREEN FOR TYPE 2 DIABETES”
ROBERT L. BARBIERI, MD (EDITORIAL, JUNE 2012)
I agree—We need to aggressively test for diabetes and lipids
I wish to commend Dr. Barbieri for his excellent discussion and recommendations for diabetic screening.
With occasional exceptions, I order a hemoglobin A1c (HbA1c) test on every patient at the time of her annual exam. If the HbA1c concentration is 5.7 or greater, I explain that she is officially “prediabetic” and needs to understand what that means.
If the HbA1c is between 6.0 and 6.5, I order a 2-hour glucose tolerance test with insulin levels. This testing picks up a large number of women with impaired fasting glucose and impaired glucose tolerance. Some will have a normal glucose tolerance test, but their insulin levels will demonstrate significant insulin resistance. All these women need to be treated with metformin, which will significantly reduce their likelihood of becoming diabetic. I also discuss and advocate lifestyle modification, but this counseling usually does not translate to a substantial change in patients’ prediabetic conditions—which is why the metformin is necessary.