When a woman has advanced prolapse of the anterior vaginal wall, it is highly likely that she has apical prolapse as well. Consider a study by Rooney and associates that determined that clinically significant vault prolapse is present in most women who have anterior vaginal prolapse of stage II or higher.1 For that reason, suspension of the vaginal apex should be considered whenever surgical treatment of anterior wall defects is planned.
Sacrocolpopexy involves suspension of the vaginal vault from the anterior longitudinal ligament of the sacrum, using Y-shaped mesh to augment native tissue (FIGURE).2 It is an effective, durable treatment for vaginal apical prolapse. With a success rate approaching 93%, this procedure has become the gold standard for repair of vault prolapse. Among its advantages are maximization of vaginal depth and preservation of a normal vaginal axis.
Sacrocolpopexy preserves the vaginal axis
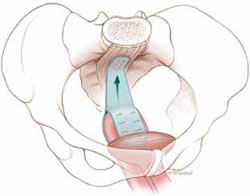
With the vaginal vault suspended from the anterior longitudinal
ligament of the sacrum, the normal vaginal axis is preserved
and vaginal depth is maximized.
Sacrocolpopexy can be performed via the abdominal, laparoscopic, or robotic-assisted approach (TABLE 1). Minimally invasive techniques are attractive because they involve faster recovery than abdominal sacrocolpopexy does. Minimally invasive techniques have also advanced to the point that they are both effective and durable. However, these advantages must be weighed against the effort required to learn the techniques, as well as their higher cost.
TABLE 1
How the 3 approaches to sacrocolpopexy compare
| Approach | Advantages and disadvantages |
|---|---|
| Abdominal | Shortest operative time No significant Trendelenburg position required Highest estimated blood loss Longest length of stay Low rate of complications Longest postoperative recovery Well-established long-term durability |
| Laparoscopic | Longer operative time Moderate Trendelenburg position required Lower estimated blood loss Shorter length of stay Surgical technique least similar to abdominal procedure Low rate of complications Shorter postoperative recovery Long-term durability less firmly established |
| Robotic-assisted | Longest operative time Steep Trendelenburg position required Lower estimated blood loss Shorter length of stay Surgical technique resembles that of abdominal approach Low rate of complications Shorter postoperative recovery Long-term durability appears to be good |
In this article, we highlight:
- a comparison of the laparoscopic and abdominal approaches to sacrocolpopexy
- an investigation of the learning curve associated with robotic-assisted sacrocolpopexy
- a study exploring the durability of robotic-assisted repair
- an estimate of the costs associated with each route of operation.
Laparoscopic vs abdominal sacrocolpopexy—how do they compare?
Paraiso MF, Walters MD, Rackley RR, Melek S, Hugney C. Laparoscopic and abdominal sacral colpopexies: a comparative cohort study. Am J Obstet Gynecol. 2005;192(5):1752–1758.
When surgeons at the Cleveland Clinic performed a retrospective cohort study to compare laparoscopic and abdominal sacrocolpopexy, they found significantly longer operative time with the laparoscopic route, with an average difference of 51 minutes (P < .0001). However, the laparoscopic approach was associated with lower blood loss (although there was no difference between groups in hematocrit on postoperative day 1); shorter hospital stay (average of 1.8 days versus 4 days [P < .001]); and comparable rates of intraoperative and postoperative complications.
Details of the trial
Paraiso and colleagues reviewed the medical charts of 56 consecutive patients who had undergone laparoscopic sacrocolpopexy, comparing them with the charts of 61 consecutive patients who had undergone the procedure using the abdominal approach. The operations had been performed between 1998 and 2003 for treatment of posthysterectomy vaginal prolapse.
The groups underwent similar rates of concurrent procedures. The laparotomy group had a significantly higher number of Burch procedures (P = .007), and the laparoscopic group had a significantly higher rate of adhesiolysis (P = .002).
Among the complications noted— which occurred at comparable rates between groups—were cystotomy, enterotomy, need for transfusion, deep-vein thrombosis, ileus, small bowel obstruction, wound infection, ventral hernia, mesh erosion, and recurrent prolapse. One laparoscopic case was converted to laparotomy because of excessive bleeding during the rectopexy portion of the operation.
Laparoscopy may have taken longer than this trial suggests
This study is one of very few well-designed trials comparing laparoscopic sacrocolpopexy to the historical gold standard of abdominal sacrocolpopexy for vault prolapse.
Twenty-eight percent of laparoscopic procedures in this study used tacking devices in lieu of suturing. Had suturing been performed universally, an even greater difference in surgical time may have been observed.

