Read Dr. Cox’s recommendations onhow to counsel women about their HPV test results in the 2011 Update on Cervical Disease.
Dr. Cox is a consultant to Gen-Probe, OncoHealth, and Roche, and serves on the Data and Safety Monitoring Committee (DSMB) for Merck HPV vaccine trials. He is a speaker for Bradley Pharmaceuticals.
The American Cancer Society estimates that approximately 12,700 new cases of invasive cervical cancer were diagnosed in 2011 in the United States; nearly 4,300 of those women will die of the disease, the Society projects.1 Great disparities in prevalence and incidence persist, with the rate of cervical cancer 1) highest in Latino women and 2) about 50% higher in African-American women than in non-Latino white women.
Because approximately 60% of cervical cancers occur in women who don’t undergo any screening for the disease, or who undergo only very infrequent screening, bringing more women in to be screened is most important. For women who are screened very infrequently, providing testing with the longest interval that provides safety should also reduce their risk of cancer.
Two advances have the potential to provide huge benefit in reducing the risk of cervical cancer: 1) increasing utilization of human papillomavirus (HPV) testing with Pap testing (so-called co-testing) for screening women 30 years and older and 2) widespread administration of the HPV vaccine to girls before they begin sexual activity. Regrettably, the promise of the HPV vaccine has not yet been fulfilled: Vaccine uptake (all three doses) among the primary target population hasn’t even reached 40%. And co-testing continues to be underutilized—in part because the best management strategy for women who have a negative Pap test result but a positive HPV test result (written here as “Pap–/HPV+”) has been less than clear.
Disappointments aside, 2011 did bring us a wealth of data on 1) the likely value of co-testing in preventing cervical cancer, and 2) improved management strategies for Pap–/HPV+ women—the areas of practice that I’ve made the focus of this year’s Update. The first question to ask: Does co-testing reduce the risk of cervical cancer more than current screening strategies that employ the Pap test?
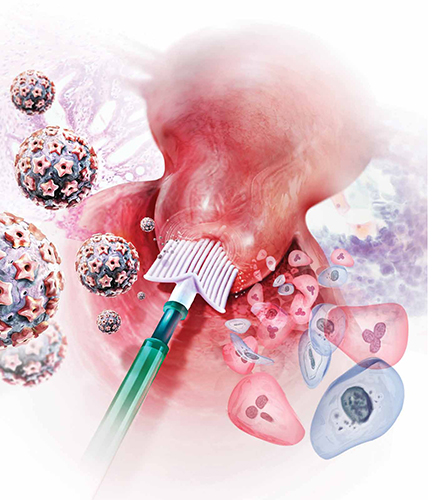
Primary cytology (Pap test) screening (above) augmented by HPV testing—so-called co-testing—appears to cut the long-term risk of cervical Ca. Consider making a co-testing stratagem part of your practice, urges author Dr. J. Thomas Cox.
Will co-testing reduce the rate of cervical Ca to a greater degree than Pap screening has?
Kinney W, Fetterman B, Cox JT, Lorey T, Flanagan T, Castle PE. Characteristics of 44 cervical cancers diagnosed following Pap-negative, high risk HPV-positive screening in routine clinical practice. Gynecol Oncol. 2011;121(2):309–313.
Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13(1):78–88.
Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12(7):663–672.
Recent studies have brought us closer to answering this question—and data certainly appear to suggest that the answer is “Yes.” Evidence from randomized controlled trials, prospective long-term cohort trials, and a large US screening population show that introducing HPV testing into cervical cancer screening could reduce cervical cancer incidence in women age ≥30—and even cervical cancer mortality.
I discussed one of these trials—the Italian NTCC trial—in the 2011 OBG Management Update on Cervical Disease [read that article in the archive at www.obgmanagement.com]; earlier detection and treatment of cervical intraepithelial neoplasia grade-3 (CIN 3) lesions in the first screening round in the co-tested group were proposed as the reasons that no cancers were detected in the second screening round (nine cancers were detected in the women having cytology only).2
Similar results were reported in the POBASCAM study from the Netherlands, in which more than 44,000 women were randomized to co-testing or screening with cytology alone, then re-screened 5 years later. As in the NTCC trial, more cases of CIN 3+ were detected and treated at the initial screen by co-testing than by cytology alone (i.e., projected out to 79 additional cases of CIN 3 and 30 additional cancers for every 100,000 women screened), with fewer cases of CIN 3+ detected in the co-tested group in the subsequent 5 years than in the cytology-only group (again, projected out to 24 fewer cases of CIN 3 and 10 fewer cancers for every 100,000 women).
(In a review of these study findings, experts at the National Cancer Institute [NCI] estimated that co-testing in POBASCAM reduced the risk of cervical cancer to only 2.2 cancers for every 100,000 women a year—demonstrating the safety of a 5-year screening interval.3) This means that women testing Pap–/HPV–, who are best screened at 3-year intervals, would be safe with an interval as long as 5 years—providing greater protection for irregularly screened women.


