Adolescents, nulliparous women, and the IUD
The professional journals scattered on your desk every month always seem to have a review article, or a study, on “long-acting reversible contraception” (LARC)—and you’re not certain why. More and more, your younger patients are asking about intrauterine devices and contraceptive implants, but you’re unsure about the most up-to-date information on the safety of these methods in adolescents. Nulliparous women are inquiring about contraception with, for one, the levonorgestrel-releasing intrauterine system (LNG-IUS; Mirena), but the Mirena package insert tells you that they are not candidates for the method.
Does this sound familiar? How do you sort through all data and advice on IUD use in adolescents and nulliparas?
Fortunately for clinicians, a great deal of research in the last few years has focused on these topics. Recommendations and reviews have been published, and public health agencies have developed easily accessible guidelines for reference.
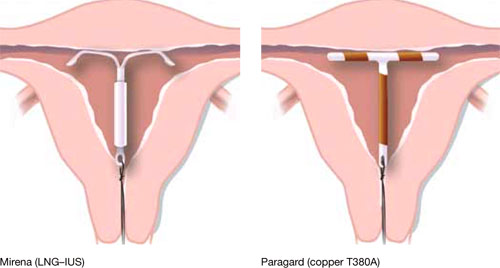
Our goal in this year’s installment of the Update on Contraception is to familiarize you with the evidence and ease any confusion, even misgivings, you might have about the two intrauterine devices available in the United States, the copper T380A (Paragard*) and Mirena* (FIGURE), especially in regard to their use in adolescents and nulliparous women.
*For ease of discussion only, we call these two systems by their brand names throughout.
FIGURE Two intrauterine devices for long-term contraception
There is real need for long-acting reversible contraception
The public health perspective
Consider these statistics about adult and adolescent women:
- Approximately 3 million pregnancies annually in the United States are unintended
- In almost half of those pregnancies, the woman undergoes an abortion
- Approximately one half of all US women have an unintended pregnancy by 45 years of age
- Given current statistics, nearly one third of all women will have chosen abortion by 45 years of age
- 80% of pregnancies in adolescents are unintended; 45% end in abortion
- 54% of women who have an abortion used a contraceptive method during the month they became pregnant—generally, a condom or an oral contraceptive.1,2
Patients’ perspective
More and more, adolescent women and nulliparous women request an IUD. Indeed, recent studies show that these populations are interested in the long-term protection that an IUD offers, and are likely to be more compliant with the method. Recent data from the National Survey of Family Growth showed an increase in IUD use in the United States: 5.5% of women who use birth control use an intrauterine device, and 14% of women who choose an IUD are adolescents.
A review of IUD use in adolescents found that, across six cohort studies and seven case reports, the continuation rate with an IUD after 1 year ranged from 48% to 88%—similar to, or better than, what is seen with oral contraceptives (OCs).3 Furthermore, two recent studies3,4 showed that:
- young nulliparous and parous women exhibit a positive attitude toward IUD use once they have been counseled on the risks and benefits of the device
- they desire effective long-term contraception
- more than 50% of the women who were surveyed thought positively about IUDs after being educated about them.
Intrauterine contraceptive use in the United States is very low compared to the rates in other developed countries—as noted, the rate here is 5.5%, for both types of IUD. Contrast that rate with what is documented in other nations: France, 20%; China, 34%; and Norway, 24%, for example. Across the developed world, IUD use is at 7.6%; in developing nations, the rate is even higher: 14.5 %.5,6
Women in the United States use the most effective forms of birth control at lower rates than the rest of the developed world; conversely, they choose permanent sterilization at a higher rate. When American women were asked, they expressed a desire for longer-acting contraception that is easy to use. Yet, they fail to take advantage of the options—often, because they lack information about them or have received erroneous education.2
Indeed, when providers of contraceptive services have been surveyed about barriers to IUD use, they point to women’s misconceptions about the devices and express their own concerns about the incidence of pelvic inflammatory disease (PID) and infertility; difficulty of insertion; and expulsion.

