- Metformin’s role in treatment of PCOS varies with the patient’s chief complaint, clinical characteristics, and lifestyle.
- The primary uses of metformin in treating PCOS are to induce ovulation in women resistant to clomiphene alone and to treat oligomenorrhea in women who can’t or won’t use oral contraceptives.
- To be a candidate for metformin treatment, a patient must have a serum creatinine lower than 1.4 mg/dL to avoid the risk of developing lactic acidosis.
Inducing ovulation. Decreasing insulin resistance. Facilitating weight loss. These are a few of the benefits metformin offers women with polycystic ovary syndrome (PCOS). This article’s 5 case histories illustrate a range of major complaints and secondary factors to consider in making prescribing decisions.
The decision to use metformin depends on the patient’s major PCOS-related complaint (TABLE 1), as well as other considerations. In some cases, metformin may not be appropriate at all.
(For dosing and common side effects, see “Metformin: The prescribing basics,”1-3)
Metformin, which is an oral biguanide unrelated to the sulfonylureas, has the potential to correct:
- Anovulatory infertility. Used alone, metformin induces ovulatory cycles in many cases. In patients with clomiphene-resistance, it can be added to the regimen to enhance ovulation rates.
- Oligomenorrhea. Although oral contraceptives remain the first-line agent, metformin is a second-line agent that restores normal menstruation in about 50% of treated women.
- Obesity. Clinical trials indicate that metformin may add helpful pharmacologic support to a diet and exercise program.
- Gestational diabetes. Early evidence suggests that use of metformin in pregnancy may reduce the incidence of gestational diabetes and spontaneous abortion, although more study is needed.
More study also will be necessary to understand the role of metformin in the treatment of hirsutism.
TABLE 1
First- and second-line therapy for the chief complaints of PCOS
| COMPLAINT | FIRST-LINE THERAPY | SECOND-LINE THERAPY |
|---|---|---|
| Oligomenorrhea | Oral contraceptive | Metformin |
| Hirsutism | Oral contraceptive plus an anti-androgen (eg, spironolactone 100mg) | Metformin plus an anti-androgen |
| Anovulatory infertility | Clomiphene or metformin alone | Clomiphene plus metformin |
| Obesity | Lifestyle changes: Increased exercise Decreased calorie intake | Metformin plus lifestyle changes |
Characteristics of PCOS
According to a group of experts working with the National Institutes of Health (NIH), polycystic ovary syndrome is the presence of oligomenorrhea or amenorrhea with clinical or laboratory evidence of hyperandrogenism (hirsutism, elevated free testosterone) in the absence of other causes such as a testosterone-producing ovarian tumor or nonclassical adrenal hyperplasia (21-hydroxylase deficiency). Using the NIH definition, a diagnosis of PCOS is not appropriate for women with regular ovulatory menses. Many authorities believe the combination of regular ovulatory menses and hirsutism should be diagnosed as idiopathic hirsutism.
The prevalence of PCOS in women of reproductive age is 4.7% in the southeastern United States; prevalence is similar in several other parts of the world where it has been measured.4-6
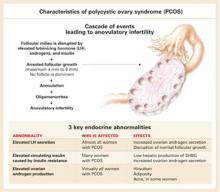
Three key endocrine abnormalities characterize PCOS:
- Elevated luteinizing hormone (LH) secretion—seen in almost all women with PCOS.7-9
- Increased circulating insulin caused by insulin resistance, found in many women with PCOS.10,11
- Elevated ovarian androgen production—present in virtually all women with PCOS. Increased androgen production causes hirsutism and, in some women, acne.
These abnormalities prevent growth of a dominant follicle (FIGURE 1), leading to anovulation and oligomenorrhea.
CASE 1
Combating PCOS-related oligomenorrhea
The primary care doctor of a 25-year-old student has established a PCOS diagnosis based on the patient’s report of 2 menstrual periods per year and an elevated serum free-testosterone measurement. Her body mass index (BMI) is 24.5, and her main problems are hirsutism, oligomenorrhea, and a propensity for gaining weight. She took the birth control pill and believes it was responsible for a 25-lb weight gain. When the patient discontinued the pill, she lost 20 lb, and she is adamantly opposed to taking it again. The patient’s pelvic examination is normal, with no evidence of virilization. She read about metformin on the Internet and asks if you will prescribe it for her oligomenorrhea.
FIGURE 1
Oral contraceptives remain first-line treatment
Metformin may be effective in some women for the treatment of oligomenorrhea. However, as mentioned earlier, more study is needed into its effects on hirsutism.
Oligomenorrhea. No large-scale clinical trial evaluating the efficacy of metformin for oligomenorrhea in women with PCOS has been reported. However, a number of smallscale clinical trials and case series suggest that metformin restores normal ovulatory menses in some women. For women with PCOS treated with metformin alone, about 25% begin regular menses within 3 months,12,13 and about 50%14 to 95%15,16 begin regular menses within 6 months. In my practice, about 50% of women begin having regular ovulatory menses after 6 months of treatment.
Patient characteristics that predict successful induction of regular ovulatory menses are not fully delineated. It appears, however, that women with elevated serum testosterone have a greater response to metformin.17