The author reports no financial relationships relevant to this article.
- Intrapartum hypoxia, once considered an important cause of cerebral palsy (CP), is responsible for only 8% to 10% of cases.
- Increasingly, evidence suggests that the primary cause of CP lies in the relationship among intrauterine infection and inflammation, preterm labor, preterm premature rupture of membranes (pPROM), and neonatal white matter disease.
- This review focuses on that relationship and its implications for managing preterm birth with intact membranes or pPROM.
Cerebral palsy is a complex disease characterized by aberrant control of movement or posture that results from an insult to the developing central nervous system (CNS). In addition to motor abnormalities, some patients have seizures, cognitive impairment, and extrapyramidal abnormalities.
Clinical and epidemiologic evidence points to white matter lesions and severe intraventricular hemorrhage (IVH)—detected by neonatal neurosonography—as the key determinants of CP. The lesions are the sonographic antecedent or counterpart of periventricular leukomalacia (PVL), a cerebral lesion characterized by foci of necrosis in the white matter near the ventricles (FIGURE).
The principal risk factor is prematurity
A precise cause for CP has not been identified in more than 75% of cases. The leading identifiable risk factor is prematurity. The prevalence of CP at 3 years of age is 4.4% among infants born earlier than 27 weeks of gestation, compared with 0.06% among babies born at term.1
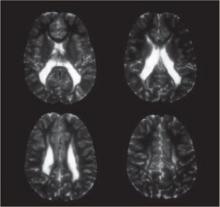
FIGURE Periventricular leukomalacia
Four axial magnetic resonance images of the brain of an infant show the usual appearance of this cerebral lesion, characterized by foci of necrosis of white matter near the ventricles.
How inflammation leads to premature birth
Any condition that increases the incidence of prematurity can be expected to increase the incidence of CP. More than 80% of premature births follow preterm labor or pPROM. Clinical and experimental evidence suggests that most of these births reflect one or more of four major pathogenic processes, which lead to uterine contractions and cervical changes, with or without premature rupture of membranes2:
- local or systemic inflammatory immune response
- activation of the maternal or fetal hypothalamic–pituitary–adrenal axis
- decidual hemorrhage (abruption)
- pathologic distention of the uterus.
Two or more of these processes often occur simultaneously, ultimately converging on a final common biochemical pathway that leads to degradation of the extracellular matrix in the cervix and fetal membranes and activation of the uterine myometrium. This process leads in turn to cervical dilation, rupture of membranes, and uterine contractions.
The “inflammatory pathway” is activated in most cases of spontaneous preterm labor and pPROM. As many as 50% of women with preterm labor and intact membranes have histologic chorioamnionitis; the rate is even higher in pPROM. The incidence of chorioamnionitis increases with decreasing gestational age.
Invading microorganisms in gestational tissues often cause intrauterine inflammation and preterm birth. Highly sensitive molecular techniques detect bacteria in the amniotic fluid of as many as half of patients with preterm labor with intact membranes3 and even more women with pPROM. As with chorioamnionitis, the lower the gestational age, the higher the bacterial isolation rates—45% at 23 to 26 weeks compared with 17% at 27 to 30 weeks.4 The microorganisms isolated are often those colonizing the vagina—most commonly anaerobes, gram-negative rods, Gardnerella vaginalis, group B streptococci, Mycoplasma hominis, and Ureaplasma urealyticum.
Infection doesn’t always lead to inflammation
Bacterial products—particularly endotoxin, a major constituent of gram-negative bacteria—bind to a specific pattern-recognition receptor, known as a toll-like receptor, on cell surfaces. This activates innate immunity and stimulates a proinflammatory immune response. Endotoxin is a potent stimulant for proinflammatory cytokines such as interleukin (IL)-1 and tumor necrosis factor (TNF)-α, which promote the release of chemoattractant cytokines such as IL-6 and IL-8. Different white blood cells migrate into the inflamed tissue and become activated at the same time.
The uterine cavity is thought to be sterile, and microorganisms there are universally associated with inflammation. Recent studies challenge this assumption. One found bacteria in as many as 90% of endometrial samples from nonpregnant women, but histologic endometritis in only 40%.5 Another noted bacteria in as many as 80% of gestational tissues delivered electively by cesarean section at term or before 32 weeks because of preeclampsia, but histologic assessment showed no or minimal inflammation.6