- Lymphatic mapping identifies the sentinel node—the node most likely to contain metastatic disease—in patients with primary solid tumors.
- In lymphatic mapping, a dye or other material that can be detected in a regional lymph node is injected at a site adjacent to the primary tumor.
- Lymphatic mapping can identify the sentinel node in 90% to 95% of patients with solid tumors, with a false-negative rate of less than 5%.
- Along with breast-conserving surgery, sentinel node biopsy is becoming a standard element of the surgical treatment of early breast cancer. It also is used in the treatment of vulvar and cervical cancers.
Not all regional lymph nodes surrounding a primary solid tumor have the same likelihood of containing metastatic disease. Rather, 1 node or a small group of nodes is at highest risk by virtue of a direct lymphatic connection to the tumor. These lymph nodes are identified by a procedure called lymphatic mapping. Mapping techniques involve the injection of a dye or other material that can be detected in a regional lymph node at a site adjacent to the primary tumor. The lymph node identified using this technique is termed the “sentinel” node (Figures 1 to 3).
Figure 1
Stage II squamous carcinoma of the vulva involving midline.
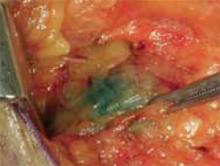
Figure 2
Peritumoral injection of isosulfan blue. The dye is taken up immediately by the cutaneous lymphatic channels.
Figure 3
Blue-stained sentinel node. The dye remains visible for 30 to 45 minutes.
A brief history
The Halstedian model of cancer surgery, introduced at the beginning of the 20th century, was a dramatic improvement over previous local surgical procedures. This model required removal of the primary tumor, the afferent lymphatic channels with the surrounding skin and fat, and all the regional lymph nodes. Procedures following Halstedian concepts—e.g., radical mastectomy with axillary lymphadenectomy and radical vulvectomy with inguinal femoral lymphadenectomy—cured many patients who otherwise would have suffered painful deaths due to locally advanced disease.
The Halstedian model was based in part on cadaver studies. These studies involved the injection of heavy metals such as mercury into lymphatic channels, followed by tedious dissection to locate both the lymphatic channels and the regional lymph nodes. At the time of these studies, no in vivo anatomic studies had been conducted; therefore, each lymph node in a regional nodal basin was thought to have an equal chance of containing metastatic disease. Thus followed the principle that all regional lymph nodes needed to be removed as part of cancer treatment.
The incidence of false-negative sentinel nodes is low—less than 5% of patients with positive nodes.
Small in vivo studies of lymphatic anatomy were begun in the mid-20th century. Zeit and Wilcoxon used cervical injections of India ink to help identify pelvic nodes in patients undergoing radical hysterectomy.1 Eichner and associates intraoperatively injected ions of blue dye into various gynecologic sites and documented in vivo drainage patterns of the reproductive organs.2-5 Parry-Jones used in vivo lymphatic mapping to correct errors in the classical anatomists’ description of the paths of vulvar lymphatics.6
Riveros et al were the first to describe the modern concept of lymphatic mapping and sentinel node biopsy.7 Since they treated many patients with advanced penile cancers, these Paraguayan urologists were seeking a technique to reduce the extent of groin dissection. They performed penile lymphography by injecting a blue dye into the phallus and cutting down to the dorsal lymphatic of the penis. They cannulated this vessel and injected ethiodized oil. When the oil was taken up in a lymph node, it could be imaged by plain radiography and was designated as the sentinel node. Cabanas studied this technique in a series of more than 70 patients and found that a negative sentinel node accurately predicted that all the remaining regional nodes were negative.8
It has not yet been determined whether patients with negative sentinel nodes can safely be spared further axillary treatment.
The sentinel node concept languished until the early 1990s, when investigators sought new ways of addressing the surgical treatment of cutaneous melanoma. One problem they faced was related to lesions at sites with ambiguous lymphatic drainage, e.g., melanomas adjacent to the umbilicus, which can drain to the groins or the axillae. Morton and colleagues utilized a procedure called lymphoscintigraphy to determine the lymphatic drainage patterns of these lesions and ascertain the appropriate target for surgical dissection.9 In lymphoscintigraphy, a small amount of radionuclide is injected near the lesion. This radionuclide is transported by the lymphatics to the sentinel node and can be imaged by standard nuclear medicine scanning.