CASE 1: Short cervix in the middle trimester
During routine second-trimester ultrasonography, a 34-year-old primigravida at 22 weeks’ gestation is found to have a cervix 15 mm in length. She has no other risk factors for spontaneous preterm birth.
What steps do you take to ensure that her pregnancy progresses uneventfully to term?
Cervical length is not routinely measured in low-risk women—i.e., those without a history of spontaneous preterm birth—but a short cervix is sometimes detected during ultrasonographic imaging for other indications, as it was in this case. When a short cervix is detected incidentally, I educate the patient to watch for early warning signs of preterm labor. I also recommend pelvic rest and a sedentary lifestyle.
The rate of preterm birth declined slightly in 2007—the first decrease in more than 20 years—but the phenomenon remains the leading cause of perinatal morbidity and mortality in developed nations.1 In the United States, more than 500,000 babies each year, or 12% to 13% of all births, are delivered before 37 weeks’ gestation. Most of these births are spontaneous and involve preterm labor or premature rupture of membranes. Medical costs for a preterm newborn exceed those of a term infant by a multiple of more than 10, and the average hospitalization exceeds that of a term infant by a multiple of more than six.
In this article, I discuss the rationale and technique for ultrasonographic cervical measurement to determine the likelihood of preterm birth. I also examine the data on the short cervix in various settings, and describe strategies for cervical assessment and preterm birth prevention, including cerclage and progesterone, framing the discussion in terms of gestational age.
Accurate and reproducible measurement of cervical length depends on correct technique. Use of transvaginal ultrasonography (TVUS) limits variations between measurements to 5% to 10%, a marked improvement over digital examination and transabdominal US.
Here are the five steps involved, in the order performed:
- Ensure that the patient’s bladder is empty. This precaution is necessary to prevent dynamic, or spontaneous, lengthening or shortening of the cervix.
- Counsel and position the patient. Explain the procedure to the patient and have her assume the dorsal lithotomy position.
- Introduce the probe into the anterior vaginal fornix using real-time visualization, and obtain a mid-sagittal view of the cervix. Withdraw the probe just enough to allow the image to blur, then advance the probe just enough for the image to regain clarity. This sequence prevents the practitioner from exerting excessive pressure on the cervix, which can falsely elongate it.
- Place an electronic caliper (on-screen) at the notch that represents the internal cervical os, and another at the external os (FIGURE 1).
- Measure the distance between the notches and report the shortest of three separately obtained measurements.
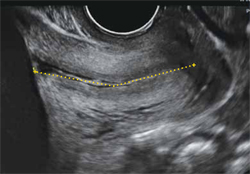
FIGURE 1 How to measure the cervix
Electronic calipers mark the internal and external os in this cervix measuring 42 mm via midsagittal transvaginal ultrasonography.
Watch for these pitfalls!
Before 20 weeks’ gestation, the lower uterine segment is not particularly well developed, making it difficult to reliably determine the location of the internal os (FIGURE 2). Moreover, focal myometrial contractions of the lower uterine segment, which are common, may give the false impression of increased cervical length or dilation of the internal os (FIGURE 2).24
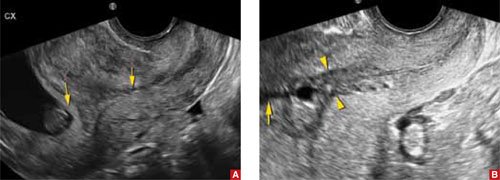
FIGURE 2 Measurement may be difficult in early pregnancy
A. This transvaginal sonogram demonstrates the difficulty of determining the location of the internal os when the lower uterine segment is undeveloped (arrows). B. When lower uterine contractions occur with the anterior and posterior walls in opposition (arrowheads), transvaginal imaging may give the false appearance of dilation with funneling (arrow).
Why we assess cervical length
In the past, the cervix was viewed as either competent—i.e., capable of maintaining a pregnancy until term—or as “incompetent.” More recent evidence has broadened our understanding of cervical function, which is now viewed along a continuum.
In landmark research in the mid-1990s, investigators compared cervical lengths, measured via transvaginal ultrasonography (TVUS), between two groups of pregnant women—those who had a history of preterm birth and those who did not.
The result? Gestational age at delivery in the first pregnancy correlated significantly—and continuously—with cervical length between 20 and 30 weeks’ gestation in the subsequent pregnancy.2 Investigators also observed that the risk of spontaneous preterm birth increased with decreasing cervical length. A length of 25 mm (10th percentile) offered a clinically appropriate threshold for identification of the risk of preterm delivery.3

