Long-acting reversible contraceptives (LARCs), which include intrauterine devices (IUDs), implants, and injectables, are being offered to more and more women because of their demonstrated safety, efficacy, and convenience. In other countries, as many as 50% of all women use an IUD, but the United States has been slow to adopt this option.1 In 2002, approximately 2% of US women used an IUD.2 That percentage rose to 5.2% between 2006 and 2008, according to a recent survey.3 In that survey, women consistently expressed a high degree of satisfaction with this method of contraception.3
So why aren’t more US women using an IUD?
A general fear of the IUD persists. Women may not even know why they fear the device; they may have simply heard that it is “bad for you.” The negative press the IUD has received in this country probably is related to poor outcomes associated with use of the Dalkon Shield IUD in the 1970s. As a reminder, the Dalkon Shield was blamed for many cases of pelvic inflammatory disease (PID) and other negative sequelae as a result of poor patient selection. In addition, some authorities believe the design of the device was severely flawed, with a string that permitted bacteria to get from the vagina to the uterus and tubes.
Today, clinicians and many patients are better educated about the prevention of chlamydia, the primary causative organism of PID and other sexually transmitted infections (STIs); patients also are better informed about safe sex practices. We now know that women should be screened for behaviors that could increase their risk for PID and render them poor candidates for the IUD.
Clinicians also have expressed concerns about reimbursement issues related to the IUD, as well as confusion and difficulty with insertion procedures and the potential for litigation. In this article, I address some of these issues in an attempt to increase the use of this highly effective contraceptive.
What’s available today
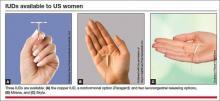
Today there are three IUDs available to US women (FIGURE):
The Copper IUD (ParaGard)—This device can be used for at least 10 years, although, in many countries, it is considered “permanent reversible contraception.” It has the advantage of being nonhormonal, making it an important option for women who cannot or will not use a hormonal contraceptive. Pregnancy is prevented through a “foreign body” effect and the spermicidal action of copper ions. The combination of these two influences prevents fertilization.4
The levonorgestrel-releasing intrauterine system (LNG-IUS) (Mirena)—This IUD is recommended for 5 years of use but may remain effective for as long as 7 years. It contains 52 mg of levonorgestrel, which it releases at a rate of approximately 20 μg/day. In addition to the foreign body effect, this IUD prevents pregnancy through progestogenic mechanisms: It thickens cervical mucus, thins the endometrium, and reduces sperm capacitation.5
The "mini" LNG-IUS (Skyla)—This newly marketed IUD is recommended for 3 years of use. It contains 13.5 mg of levonorgestrel, which it releases at a rate of 14 μg/day. It has the same mechanism of action as Mirena but may be easier to insert owing to its slightly smaller size and preloaded inserter.
Myth #1: The IUD is not suitable for teens and nulliparous women
This myth arose out of concerns about the smaller uterine cavity and cervical diameter of teens and nulliparous women. Today we know that an IUD can be inserted safely in this population. Moreover, because adolescents are at high risk for unintended pregnancy, they stand to benefit uniquely from LARC options, including the IUD. As the American College of Obstetricians and Gynecologists (ACOG) recommends in a recent Committee Opinion on adolescents and LARCs, the IUD should be a “first-line” option for all women of reproductive age.6
Myth #2: An IUD should not be inserted immediately after childbirth
For many years, it was assumed that an IUD should be inserted in the postpartum period only after uterine involution was completed. However, in 2010, the Centers for Disease Control and Prevention (CDC) published medical eligibility criteria for contraceptive use, which included the following recommendations for breastfeeding or non–breast-feeding women:
• Mirena was given a Level 2 recommendation (advantages outweigh risks) for insertion within 10 minutes after delivery of the placenta
• The copper IUD was given a Level 1 recommendation (no restrictions) for insertion within the same time interval
• From 10 minutes to 4 weeks postpartum, both devices have a Level 2 recommendation for insertion
• Beyond 4 weeks, both devices have a Level 1 recommendation for insertion.7
Immediate post-delivery insertion of an IUD has several benefits, including: