Clinical Review
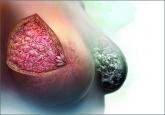
Atypical hyperplasia of the breast: Cancer risk-reduction strategies
Women with atypical hyperplasia are at increased risk for breast cancer. We need to characterize that risk for patients and ensure appropriate...

Letters from readers
Is the risk of EPT
substantially higher?
I found this article interesting, and I agree that women who have atypical hyperplasia should be counseled to consider the possible additional risk of hormone use. I didn’t see a reference, however, that supported this assertion: “Accordingly, the absolute risk of invasive breast cancer associated with use of
estrogen-progestin menopausal hormone therapy (EPT) is also likely substantially higher than in average-risk women.”
Are there any high-quality studies that support this?
Brad Logan, MD
Tampa, Florida
Adverse effects from agents that suppress estrogen levels
Are any studies being done to look at bazedoxifene in these patients alone or especially in combination with an estrogen? Encouraging the use of agents long term that profoundly suppress actual or effective estrogen levels, especially in young women, ignores the very profound adverse effects these agents can have both in the immediate and long term. I would be curious to know if there are any studies or recommendations regarding the use of gonadotropin agonists or antiandrogens in men older than age 35 to prevent prostate cancer.
Jewell E. Malick, DO
Rockwall, Texas
Drs. Kaunitz and Samiian respond
We appreciate the thoughtful letters from Drs. Logan and Malick concerning our article on atypical
hyperplasia (AH) of the breast. Regarding Dr. Logan’s question, we are not aware of any randomized controlled trials that have assessed the impact of EPT on the risk of being diagnosed with invasive breast
cancer in women with a history of AH. An observational study looking
at this issue did not distinguish between estrogen hormone therapy (ET) and EPT.1
However, we do know that in women at average risk for breast cancer, EPT increases the absolute risk of an invasive breast cancer by 1 additional case per 1,000 person- years of use.2 Accordingly, since women with a prior biopsy diagnosis of AH have a 4-fold elevated risk of being diagnosed with invasive breast cancer, it is reasonable to speculate that EPT would elevate this risk to some 4 additional cases per 1,000 person- years of use. This is why we recommend that women with a history of AH considering use of EPT be counseled regarding this potential elevated risk of being diagnosed with invasive breast cancer.
Regarding Dr. Malick’s questions, we are not aware of trials assessing the impact that bazedoxifene (with or without estrogen) has in women with a prior biopsy demonstrating AH. With respect to trials assessing androgen blockers in men to prevent prostate cancer, the Prostate Cancer Prevention Trial is assessing the use of finasteride in men aged 55 years and older.3
“UPDATE ON OPERATIVE VAGINAL DELIVERY”
WILLIAM H. BARTH JR, MD (July 2015)
With the US cesarean delivery rate hovering at 31%, it may be time to revisit forceps
(Keilland forceps in particular), says William H. Barth Jr, MD, in the July “Update on operative vaginal delivery.” More than
130 readers weighed in when asked if they agree if forceps have a place in their obstetric toolbox:
To participate in the latest Quick Poll, visit obgmanagement.com
READERS WEIGH IN:
Patients’ unrealistic expectations influence
clinicians’ decisions
We all have been trained in the use of forceps at delivery. Perhaps the fact that more than one-third of the Quick Poll votes registered “no” reflects the reluctance of providers to use forceps because of our patients’ tendencies to have unrealistic expectations about childbirth and risk. Given the marginally better outcomes, I will continue to use vacuum extraction when faced with an outlet delivery dilemma.
William White, MD
Mammoth Lakes, California
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Women with atypical hyperplasia are at increased risk for breast cancer. We need to characterize that risk for patients and ensure appropriate...

New data confirm that the combination of forceps and vacuum extraction should be avoided and demonstrate that use of midcavity rotational forceps...
What will you tell your patient who asks about the clinical significance of dense breasts detected on her mammogram? Here I offer my current...

The authors of this prospective study involving more than 350,000 patients observed high interval cancer rates for women with 5-year breast cancer...
